 Life can change at the drop of a hat, but few know it better than Ricky and his family. At just five months old, his health took a turn. What first seemed like a bad flu continued to get worse. The doctors kept running tests, prescribing medications, and referring specialists, not knowing what was wrong.
Life can change at the drop of a hat, but few know it better than Ricky and his family. At just five months old, his health took a turn. What first seemed like a bad flu continued to get worse. The doctors kept running tests, prescribing medications, and referring specialists, not knowing what was wrong.
While it was clear his body was fighting something, it took time to name the struggle. Ricky was almost a year old and still wasn’t walking. Test results revealed Ricky’s elevated muscle enzymes. After even more tests and doctor visits, they finally had a diagnosis. Ricky had Duchenne Muscular Dystrophy (DMD). Rosie was told, “Take your child home and love him. There’s nothing we can do.” She recalls, “I was just so angry. Those are not words that parents, especially not a mother, want to hear. And yet here he is 18 years later.”
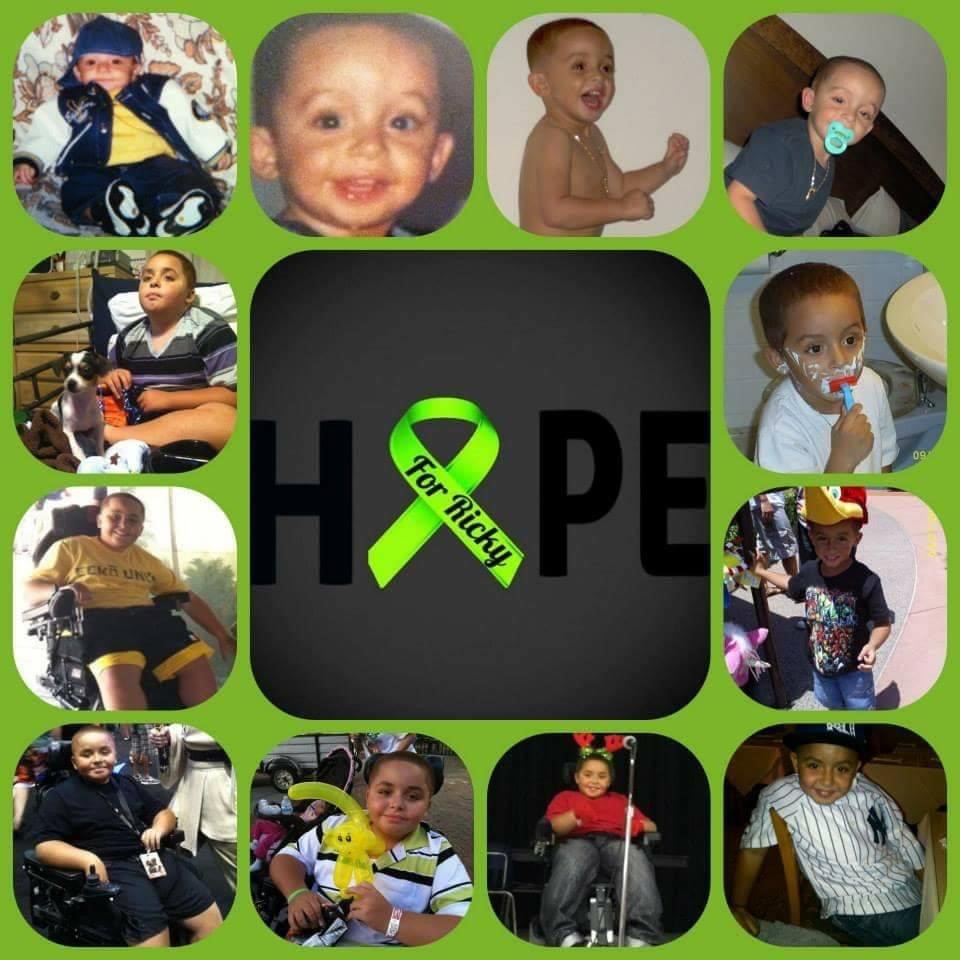 From that moment on, Rosie researched potential treatments day and night—beginning with available treatments in their home state, Florida. She came across the Muscular Dystrophy Association (MDA) and brought Ricky to their clinic.
From that moment on, Rosie researched potential treatments day and night—beginning with available treatments in their home state, Florida. She came across the Muscular Dystrophy Association (MDA) and brought Ricky to their clinic.
 By seven-years-old, he was already in a power wheelchair full time. For both Ricky and Rosie, the transition from walking to wheelchair was a challenging one. Rosie shares, “Ricky didn’t understand why he had to use it, why he couldn’t be like the other kids. I didn’t tell him everything because he was still so young, but I shared that he had muscle weakness. I didn’t want him to worry, so I left it at that.”
By seven-years-old, he was already in a power wheelchair full time. For both Ricky and Rosie, the transition from walking to wheelchair was a challenging one. Rosie shares, “Ricky didn’t understand why he had to use it, why he couldn’t be like the other kids. I didn’t tell him everything because he was still so young, but I shared that he had muscle weakness. I didn’t want him to worry, so I left it at that.”
Outside of treatment, Ricky was thriving. “At school he had a few girls in the class that just adored him,” Rosie explains. “One would walk with his book bag in front of them and then two would walk by his side. They really helped him.”
As Ricky got older, he continued seeing doctors regularly, including a new pulmonary doctor. “We had a lot of different people telling us different things,” Rosie says. “We were just so lost.” After Ricky was diagnosed with asthma, Rosie continues, “Something inside told me he just didn’t have it. His sister has asthma and their symptoms weren’t the same, but it was hard for us to push back.” Only later did they realize his worsening breathing problems were due to heart failure.
Moving Closer to Care
By the time he was 11, Ricky’s heart function and breathing worsened. His test results indicated that even though his heart was weak, it wasn’t bad enough yet to consider heart transplant. Even so, his heart health needed to be followed closely, so he visited cardiology every three months.
Then came the day that would eventually lead to their move from Florida to Ohio. Ricky remembers it well, “On December 3rd, 2017 I felt sick enough to go to the hospital.” He was dry heaving, coughing up frothy spit, and then the vomiting started. At the hospital, they were told that he had pneumonia.
That weekend, the doctor came in and closed the door behind them. His heart function was bad enough that the medical team worried he could have a dangerous heart rhythm. If so, he would need surgery to put in a defibrillator and restart his heart.. They said, “He can’t go home. He’s scheduled for surgery on Monday morning.” It would be his first real surgery. Rosie was terrified. Ricky was terrified. But they kept reassuring each other. Rosie made a promise to him: “The first face you’ll see before you go will be me. And when you wake up, it’s going to be me.”
 Though the surgery itself went well, his heart continued to get worse. The coughing wouldn’t go away. They tried to pursue a transplant, but in the end the doctors decided against it. They were going to let him go at 15-years-old. And for the second time, Rosie decided, “No, this is not it.”
Though the surgery itself went well, his heart continued to get worse. The coughing wouldn’t go away. They tried to pursue a transplant, but in the end the doctors decided against it. They were going to let him go at 15-years-old. And for the second time, Rosie decided, “No, this is not it.”
Rosie began looking into Left Ventricular Assist Devices (LVADs) for Duchenne and discovered only a few centers in the country were using them. Rosie had taken to social media about Ricky’s heart failure. A carrier with DMD saw her post and told her Cincinnati Children’s did her LVAD and that they should talk to Dr. Angela Lorts, her VAD doctor. That’s the confirmation Rosie needed.
“We had to fight to get there, with insurance, with everybody,” Rosie shares, but 5 months later they finally arrived in Cincinnati. On the second day of evaluation, Ricky was sick enough to be admitted into the cardiac ICU.
The doctors came back with some choices: we could do the LVAD surgery or take him home and they would make him as comfortable as possible. The team outlined all the good and the bad that could happen from there.
It was a really hard decision. Rosie thought it over for two weeks. It came down to Ricky. “I looked at my son and said, “I need to know what you want to do. Do you want this?” At 15-years-old, Ricky decided to go for the surgery.
Documenting the Journey
In preparation for the LVAD surgery, Rosie describes how everyone went the extra mile. “They did a simulation with a dummy, which we called “Ricky Bobby” [laughs]. We learned it was possible he could end up on a feeding tube or a ventilator for the rest of his life. He could be bed bound—that recovery was the hardest part.” Throughout the patient education, the Cincinnati Children’s DMD team became like family to Ricky and Rosie.
Still, it was difficult to be away from home and without anyone who had gone through the process before. To help others in their situation, Rosie has been active on social media for families to follow the journey.
“That’s why me and Ricky do what we do. We don’t want others to go through it alone,” Rosie says. “I always tell other families, ‘You can’t go by everything that I’ve been doing because it’s not the same for everybody’.” To Ricky and Rosie, the DMD community needs that support.
Life Post-Surgery
 Just a few days before Ricky’s 16th birthday, he went in for the LVAD surgery. Many hours later, the team and Ricky’s family celebrated the successful surgery. Recovery has been its own journey with its own set of new challenges. He has to take new medications including blood thinners that require more blood draws and diet changes. He needed to have wheelchair adjustments to help him get in and out of the chair with an LVAD. He also has more clinic visits than before so the team can make sure his LVAD is working well.
Just a few days before Ricky’s 16th birthday, he went in for the LVAD surgery. Many hours later, the team and Ricky’s family celebrated the successful surgery. Recovery has been its own journey with its own set of new challenges. He has to take new medications including blood thinners that require more blood draws and diet changes. He needed to have wheelchair adjustments to help him get in and out of the chair with an LVAD. He also has more clinic visits than before so the team can make sure his LVAD is working well.
While he sees the cardiologists much more than he used to, the LVAD improved things. Ricky’s blood flow has strengthened and his energy has increased. His breathing has improved. As Rosie puts it, “He has energy and I have a sense of calm. The LVAD keeps going, so I know his heart keeps going.”
Now, Ricky and Rosie are back home in Florida, exploring what life looks like now that Ricky is an adult with an LVAD. While the search for care and trusted medical providers is ongoing, they can now also explore and visit places they’ve wanted to go. They go to baseball games and the Star Wars park in Disneyland. To Rosie, that’s the best part: “He’s still here. He’s healed and doing well. We’re experiencing everything in life.”
ACTION, VADs and DMD
 ACTION is working to understand who may benefit the most from VAD therapy. We are also committed to patients and families, and helping them make the best decision with their care team no matter where they live. While VADs are not right for everyone, we believe everyone should know about the options and why a VAD may or may not work for them. Learn more about VADs in muscular dystrophy here.
ACTION is working to understand who may benefit the most from VAD therapy. We are also committed to patients and families, and helping them make the best decision with their care team no matter where they live. While VADs are not right for everyone, we believe everyone should know about the options and why a VAD may or may not work for them. Learn more about VADs in muscular dystrophy here.

